Menopause is a natural phase in a woman’s life, but many don’t realize its profound impact on bone health. As estrogen levels decline during menopause, bone density can decrease rapidly, increasing the risk of osteoporosis and fractures.
Understanding how menopause affects bone strength is essential for preventing long-term complications.
In this article, we explore how menopause affects bones, its health implications, and proactive ways to maintain strong, healthy bones through this significant life transition.
Why Bone Health Matters During Menopause
Bone health becomes especially crucial during menopause because this life stage accelerates bone loss, increasing the risk of osteoporosis and fractures. Declining estrogen levels significantly impact bone density, weakening the bone structure and making even minor falls dangerous.
Prioritizing bone health during menopause ensures you maintain strength, mobility, and independence as you age, preventing complications that can affect your daily life and overall well-being.
What Is Bone Density and Why Is It Important?
Bone density refers to the amount of mineral matter per square centimeter of bones, indicating their strength and health.
During menopause, bone density naturally decreases due to lower estrogen levels.
- Menopause and bone density are closely linked, as hormonal changes accelerate bone thinning.
- Low bone density increases the risk of fractures, affecting mobility and independence.
- Maintaining bone density helps reduce menopause bone loss and its long-term impacts.
- Strong bones support posture, daily movements, and protect vital organs from injury.
How Menopause Affects Bone Health
Menopause causes significant hormonal changes that directly impact bone health. The drop in estrogen levels leads to a decrease in bone density, weakening bones and increasing fracture risks. Knowing the relationship between estrogen and bone density is crucial to maintaining bone health during menopause.
- Estrogen plays a vital role in keeping bones strong and dense.
- The decline in estrogen during menopause accelerates bone thinning.
- Osteoporosis and menopause are closely linked due to hormonal changes.
- Protecting bone health during menopause reduces the risk of fractures and osteoporosis.
Risk Factors That Compound Bone Density Loss After Menopause
While menopause itself accelerates bone loss, several other factors can worsen the decline in postmenopausal bone health and increase osteoporosis risk.
Here are major risk factors to consider:
Age and Genetics
Bone density naturally decreases with age, making older women more susceptible to osteoporosis. Genetics also play a role, as a family history of osteoporosis or fractures increases your risk for low bone density.
Lifestyle Factors
A sedentary lifestyle, poor nutrition, and smoking negatively affect bone health during menopause. Lack of weight-bearing exercises and low calcium or vitamin D intake contribute to rapid bone density loss.
Medical Conditions or Medications That Accelerate Bone Loss
Certain conditions like rheumatoid arthritis or medications such as long-term steroids can worsen bone thinning after menopause. Discuss with your doctor how these factors may affect your postmenopausal bone health and explore preventive options.
Early Warning Signs of Decreasing Bone Density
Bone loss often progresses silently, but there are early warning signs you shouldn’t ignore. Monitoring your bone density test results and staying aware of physical changes are key to preventing osteoporosis.
Here are signs that may indicate declining postmenopausal bone health:
- Noticeable loss of height over time.
- A stooped posture or curvature in the upper back.
- Frequent back pain, especially in the lower or middle back.
- Fractures occurring from minor falls or movements.
How to Protect Your Bones During and After Menopause
Protecting your bones during and after menopause is essential to reduce the risk of fractures and osteoporosis. Here are key ways to maintain strong bones and learn how to prevent bone loss after menopause effectively.
Diet and Nutrition
What you eat has a direct impact on your bone health, especially during menopause. Consuming calcium-rich foods, such as dairy, leafy greens, and fortified products, helps maintain bone density. Adequate vitamin D intake is also crucial as it aids calcium absorption, preventing bone weakening.
Exercise and Strength Training
Staying active is one of the best strategies for how to prevent bone loss after menopause. Weight-bearing exercises like walking, jogging, and dancing help build bone strength. Strength training, such as lifting light weights or using resistance bands, also maintains bone density and supports overall mobility.
Medical Interventions
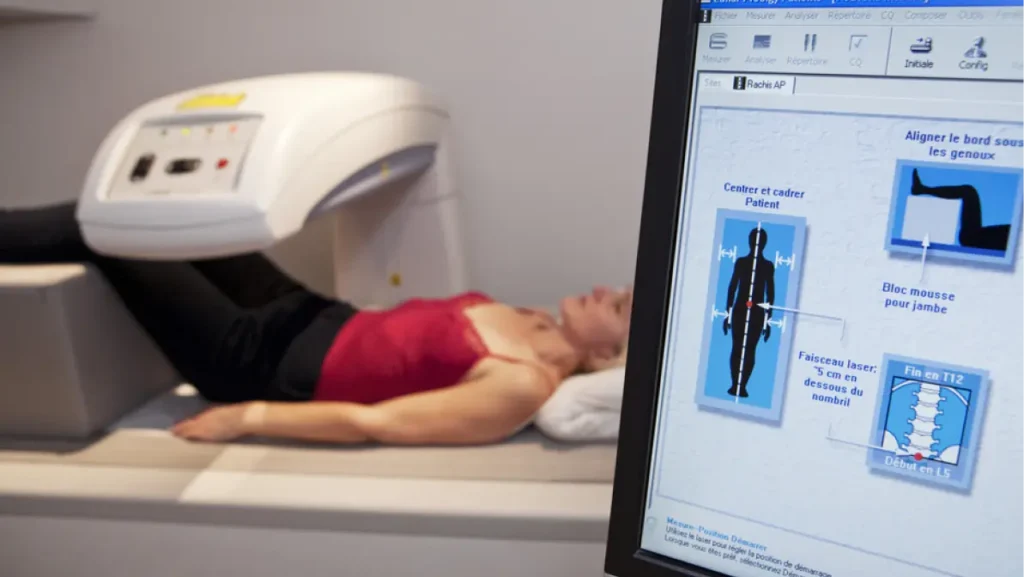
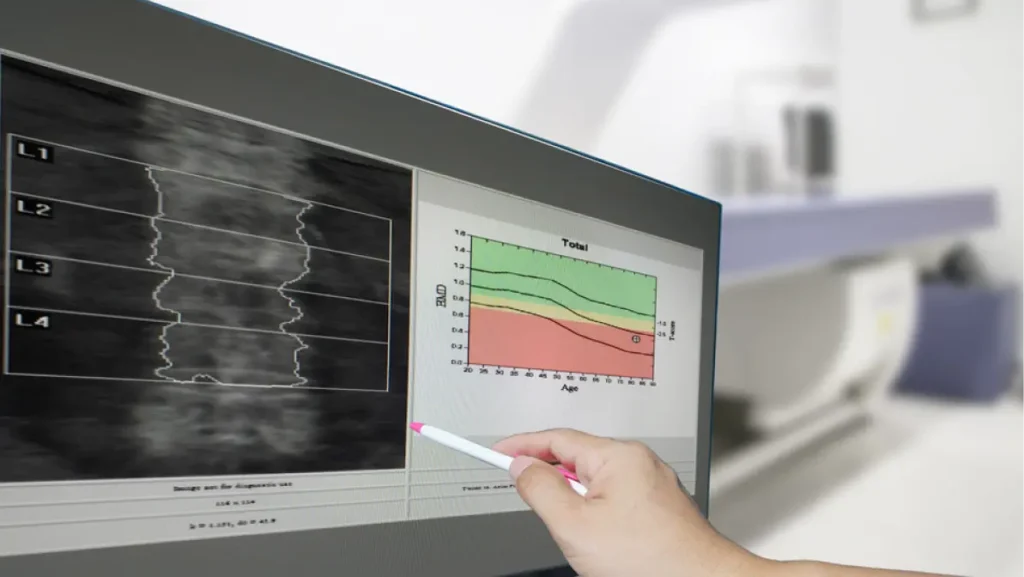
Consulting your doctor about medical interventions is vital for long-term bone health. Options include hormone replacement therapy (HRT) or medications designed to slow bone loss and build density.
Scheduling a DEX A scan for bone density assessment helps monitor bone health and guides treatment decisions.
Lifestyle Tips for Long-Term Bone Health

Maintaining healthy lifestyle habits plays a significant role in protecting your bones as you age. Here are practical tips to support your bone health for the long term.
Quit smoking and limit alcohol
Smoking accelerates bone loss and decreases calcium absorption, increasing osteoporosis risk. Limiting alcohol intake also helps protect bone density and reduces the risk of falls and fractures.
Get regular physical activity
Staying physically active keeps your bones strong and supports balance and coordination. Weight-bearing activities, yoga, and strength and pain management exercises all contribute to healthier bones and reduced fracture risks.
Maintain a healthy weight
Keeping your weight within a healthy range reduces strain on bones and joints. Being underweight increases fracture risk, while being overweight may lead to joint issues and mobility problems.
Prioritize Your Bone Health with One Step Diagnostic
Maintaining bone health during menopause is crucial to ensure strength, mobility, and independence in your later years.
With proper diet, exercise, and medical monitoring, you can confidently manage bone density changes and prevent osteoporosis.
One Step Diagnostic offers comprehensive bone health assessments, including DEXA scan for bone density, to help you understand and protect your bone health effectively. Schedule your scan today and take the first step toward stronger, healthier bones. Book your DEXA scan at One Step Diagnostic in Houston today and prioritize your bone health with confidence.