Introduction:
One of the most significant discoveries in modern medicine is magnetic resonance imaging, or MRI. Surgeons can effectively assess and identify illnesses that would otherwise have a significant impact on life with the help of MRI technology.
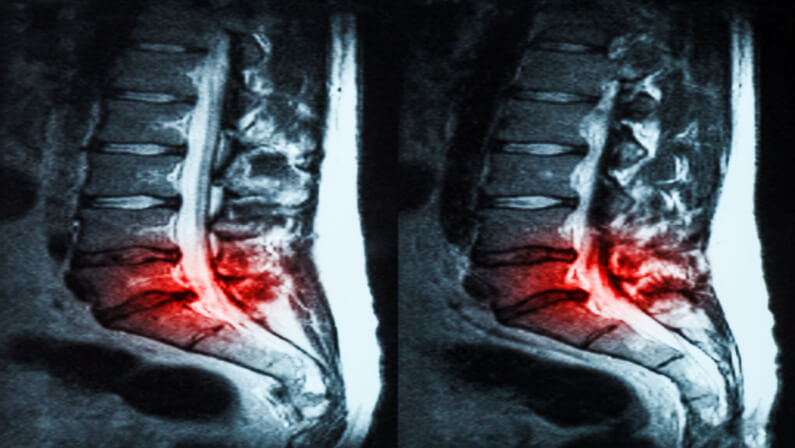
What Is a Herniated Disc MRI
Herniated discs are frequently diagnosed and monitored with MRI scans. Finding the location of the herniated disc(s) in the spine and the level of nerve compression is one of the most frequent uses for them.
Your doctor could suggest additional testing to better assess the condition if the MRI results show a herniated disc.
Diagnosing a Herniated Disc
For your doctor to figure out if you have a herniated disc, he or she will first want to know about your back pain.
It is helpful to tell your doctor as much as you can about where your back pain is coming from, what other symptoms you have, and how bad your symptoms are.
Your doctor might also do a physical exam to look at your spine and the muscles and soft tissues around it.
A herniated disc can also be seen on an MRI scan or other advanced imaging test. Your doctor may ask for an MRI to get a better idea of where the herniated disc is and how bad it is.
How to Read an MRI for a Herniated Disc
The meaning of an MRI scan depends on a number of things. As with many other diagnostic tests, the problem with MRI scan results is that the “disorder” that shows up on the scan is not always the cause of backaches.
For a patient to be able to correctly read a lumbar MRI scan for a herniated disc, they must have a basic understanding of how the lumbar spine is built.
In the lower back, there are 5 vertebrae that are connected by facet and disc joints. Most of the time, these discs are in constant motion, which causes wear and tear. When the outer layer of the disc is torn, this is called an annular tear.
When this happens, the jelly-like center of the disc squeezes out into the spinal canal, causing a hernia. An MRI scan will often show this hernia as a spot that stands out.
Herniated Disc Causes
There are 23 intervertebral discs in the spine as a whole. These discs are tissue joints between the vertebrae in the spine. They have a soft gel-like center and a firm wall on the outside (annulus fibrosus).
Sometimes, the outer wall of the disc can get a hole called an annular tear, which lets the jelly-like nucleus squeeze through. If only a small amount of the nucleus comes out of the annular tear, this is called a herniated disc or a bulging disc.
There are many things that can lead to a herniated disc. Most trauma comes from being hurt or from wear and tear.
As people get older, the cartilage that connects the spine’s discs to the vertebrae can become loose and lose its elasticity.
Herniated discs can also be caused by a sudden blow or trauma, like an accident or a fall.
Herniated Disc Symptoms
Herniated discs usually hurt nearby nerves. The annular rip is severely inflamed by the nucleus pulposus and outer annulus fibrosus’ tiny blood vessels.
Somatic afferent (SA) sensory nerves carry pain signals from the back of the disc, where a certain type of pain nerve fiber is, to the brain.
The post-central gyrus’ main somatosensory cortex receives somatic afferent (SA) fibers. This region of the brain identifies pain signals from throughout the body as “sharp” or “stabbing.”
SA pain fibers are directed to the posterior annulus, making herniated disc pain easy to pinpoint.
Most herniated discs cause sharp pain over the inflamed disc (s). Inflammation can spread to the nerve and spinal cord-protecting dural lining when a disc herniates.
Inflammation can spread to the nerve and spinal cord-protecting dural lining when a disc herniates. Cervicogenic headaches originate in the neck and progress to the back of the head.
Herniated discs can cause discomfort in the arms, legs, or ribs when inflammation extends to the nerve root covering (thoracic herniations).
Herniated disc symptoms often appear in the nerve root dermatome.
- Arms
- elbows,
- and shoulders lose feeling
This disorder, called cervical radiculopathy, causes radiating pain and heat from the source.
Disc herniation may impair nerve root myotome muscles in the arm or leg. This weakens the triceps, shoulders, legs, and upper arm. The patient may struggle to move certain body parts.
Best Treatment Options for a Herniated Disc
The top surgical procedures for herniated discs are highlighted below:
1. Laser Disc Repair
The Laser Disc Repair process involves very little physical contact. By passing through a small opening in the spine known as the neural-foramen, the surgeon uses an endoscope (a tiny tube with a light and camera attached) to access the area causing the back pain without removing any supporting joints, bones, or ligaments.
Herniated discs can cause neck or back pain, but this ground-breaking outpatient surgery has been shown to be effective in treating both conditions. Utilizing only FDA-approved technologies, this operation has been shown to be both safe and successful.
After visualizing the injured disc using a small endoscope, the surgeon utilizes a precise laser to remove only the damaged disc tissue that is causing the pain. The precision laser will not harm the nearby bone or tissues because the wounded tissue makes up only 5 to 10% of the total disc tissue, protecting the healthy disc.
2. Spinal Fusion Surgery / Spinal Arthrodesis
During a spinal fusion operation, the surgeon joins or “fuses” two or more vertebrae together for good. When these vertebrae fuse together, they become one solid, long bone, but they can no longer move naturally. This surgical procedure was made to look like how broken bones heal on their own.
Bone grafts can be taken from a patient’s hip during surgery, a bone from a dead person, or they can be made ahead of time. For fusion to happen, usually bone grafting and metal implants are needed. Recently, more than 100 people who got bone grafts for fusions got Tuberculosis from the bone grafts. This unfortunate event showed how invasive types of spine surgery, like spinal fusion and artificial discs, can cause serious problems.
When a surgeon does spinal fusion, they take out the entire disc, put a bone graft between the painful vertebrae, and then fuse the vertebrae together to make one solid piece. This solid unit stops the painful vertebrae from moving, but the loss of movement is permanent. Complications are common, and they can be very bad or even kill you.
3. Discectomy Surgery
During a discectomy, the herniated part of a damaged disc on the outside is removed. This relieves pressure on the nerve roots. It doesn’t help with back or neck pain.
Instead, it helps with leg or arm pain. The surgeon does this by going into the back of the patient and making holes in the spine’s bones and ligaments to get to the herniation.
The surgeon uses different tools to cut through the tissues around the vertebra. He or she then removes bone, ligament, and part of the herniated part of the disc. Surgeons can only remove as much of the herniation as they can see.
Since they can’t see all of the herniation during a discectomy, they only remove a small amount of the herniation. This is the main reason why this procedure doesn’t work well, and why Deuk Spine Institute doesn’t do it.
A discectomy means “cutting out the disc,” and in one treatment, a patient can have one or more discs taken out. Different sets of vertebrae are called “levels.” When a discectomy is done, the “open” method is used. The surgeon makes a wider cut, which is more invasive than the minimally invasive procedure, so he or she can see the spine directly.
Due to the tools used to make the incision and do the operation, as well as the fact that it is hard to see what is going on, there is a high risk of infection and nerve damage to the nerve roots near the incision. This is an older method that doesn’t use newer, more advanced tools like the endoscope or microsurgery.
4. Microdiscectomy Surgery
Microdiscectomy is quite similar to discectomy surgery. It involves a microscope and a 2–3-inch skin incision. A microdiscectomy removes out-of-place disc material that presses on nerve roots. The surgeon cuts the patient’s back 2–3 inches above the herniated disc.
After cutting muscle from the spine, the surgeon removes bone and ligaments to reach the hernia. Sciatica patients employ this method. This procedure worsens back pain. Many people who have a microdiscectomy have their symptoms return within a year or two and need further procedures to repair the damage.
5. Artificial Disc
Candidates for artificial disc replacement often experience ongoing arm or leg discomfort despite physical therapy and medications. The doctor removes the damaged disc and replaces it with a metal or plastic implant during artificial disc surgery.
A synthetic disc that operates like a natural disc replaces the damaged disc. Surgeons can reach the spine via repositioning sensitive organs in the patient’s neck or belly. Many surgeons and patients avoid anterior (through the belly) spinal surgery for lumbar disc problems since it is one of the most difficult and risky approaches.
After a synthetic disc replacement, patients should expect to stay in the hospital for two to three days before going home. Within 24 hours of surgery, individuals can walk. The goal is to alleviate pain while retaining disc motion, unlike fusion.
How Long for a Herniated Disc to Heal Without Surgery?
Herniated discs frequently recover on their own. These wounds recover in a few days or, at most, four weeks. In over 90% of cases, a herniated disc is minor and doesn’t need surgery.
In some situations, simple therapies like a few days of good rest and a few weeks of temporary lifestyle modifications will be sufficient to relieve the symptoms of a herniated disc. Symptoms frequently completely diminish for patients within a few weeks or even days.
Laser Disc Repair should be performed on the patient if the patient experiences discomfort or symptoms from a herniated or bulging disc for more than four weeks.
If you wait much longer, your body’s other muscles and joints will degrade and start to malfunction, causing more pain. Surgery should not be delayed for longer than 1-2 months after the onset of symptoms because doing so worsens the patient’s condition and reduces life expectancy.
Key Takeaways
There are times when performing different physical exercises might help relieve the pressure caused by a herniated disc on a nerve root. Regardless of prior fitness experience or history, anyone can perform the variously demanding workouts.
Because they inflict the least amount of pain and suffering while targeting specific muscle regions, low-impact exercises are especially advised.
One Step Diagnostic is a radiology center that has received accreditation from the American College of Radiology (ACR). It has numerous locations across Texas, including five clinics in Houston and additional sites in Sugarland, Dickinson, and The Woodlands. To guarantee that their patients receive the best care possible, the clinic only hires radiologists who have received board certification. Call us for more information on how we can help you.